Cancer Immunology Program
The Cancer Immunotherapy Program at CSB, directed by Christopher Garris, PhD, is focused on the major goals of (1) deciphering the mechanisms of tumor immunogenicity, (2) expanding the scope of analytical methods to assess tumor immune interactions, and (3) developing novel anti-cancer therapeutics.
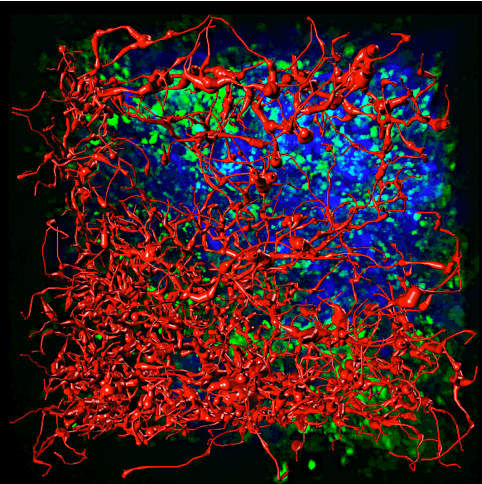
We have assembled a team of labs at MGH ( Weissleder, Pai, Hwang, and Garris) with diverse yet complementary research backgrounds who conduct basic and translational cancer immunology research. We combine advanced in vivo imaging, cancer immunotherapy, nanotherapeutics, bio-orthogonal chemistry, neuroimmunology, genomics, and drug development approaches into a comprehensive, collaborative research program. Our extensive technological expertise includes: in vivo cancer models, spatial proteotranscriptomics, 3D co-cultures, genetic engineering, patient-derived histocultures, and highly multiplexed flow cytometry and imaging. Our cancers of interest include head and neck, glioblastoma, pancreatic, bladder, and melanoma. To support these investigations, we have established biobanks of human cancer samples to curate salient features of human disease. We have designed a repertoire of mouse cancer models for proof of concept studies of novel therapeutics. These are used for mechanistic testing of drug activity through our long-term initiative to monitor anti-tumor immune responses in situ.
In line with our major goals, we have established 3 pillar sub-programs for the CSB Cancer Immunology Program.
- Fundamental Discovery - Focusing on fundamental tumor-immune interactions, we seek to distill properties of tumor immune recognition through defined mechanisms. Studies utilizing the mouse as a model system, or primary profiling of human tissues
- Comprehensive Immune Monitoring - Development of new methods to explore immune function in vivo and in longitudinal analysis of treatment response. These studies enable not only enhanced characterization of the tumor microenvironment, but also define the mechanisms of action of therapeutics developed in the Therapeutics Initiative.
- Translation of Innovative Therapeutics - Using information derived from programs 1 and 2, we create novel therapeutics to treat cancer. Platforms designed in program 2 can then be used to define biomarkers of response and refine therapeutic dosing and indications
Research Projects
Tumor microenvironment
The growth of a tumor and its ability to progress and metastasize is influenced by a variety of host components, including various stomal and immune cells. Precisely how the microenvironment influences tumor outgrowth remains poorly understood. This Program utilizes recent advances in molecular imaging, nanoscale materials and gene profiling efforts to quantify and model cellular and molecular immune components of the tumor microenvironment. The approaches are aimed to discover fundamental aspects of immune responses to cancer and establish new paradigms for future translational efforts. Additionally, the Program investigates tumor-driven mechanisms that modulate immune cells in the entire body. This important considering that some tumors affect immune cell components well beyond the local tissue microenvironment and that immune cell subsets in various body compartment can regulate tumor cell dissemination and metastasis.
Immunotherapy
The first wave of immuno-oncology therapies has revolutionized cancer treatment by successfully demonstrating that enhancing antitumor T cell activity controls some cancers durably and provides impressive survival benefits. Considering that tumor microenvironments are home to diverse immune cell types, including cells other than T cells, it is a critical time to uncover whether additional immune components are relevant next generation immuno-oncology targets. This Program specifically explores ways for stimulating both adaptive and innate antitumor immunity, and methods for rationally identifying effective new drug combinations. The Program also uses new reporters and imaging tools to uncover how drugs affect immune cells in real time in vivo. By considering multiple immune cell types and examining drug response and resistance mechanisms, the Program aims to define new therapeutic interventions that stimulate immunity against a broader diversity of tumors and improve the quality of life of more patients. Targeting resistance barriers contributed by several tumor-associated host components may be particularly relevant for patients who resist T cell immune checkpoint blockade treatments.
Recent Publications
Zitti B, Duval F, Wirapati P, Hicham M, Xie Y, Oh J, Hoelzl J, Meiser P, Varrone M, Peterson HM, Cianciaruso C, Bill R, Bayerl F, Bolli E, Goubet AG, Kiss M, McDowell S, Cheng P, Celestini D, Terzic J, Zwahlen T, Alouche N, Zouggari N, Tarussio D, Tissot S, Nunes-Hasler P, Mino-Kenudson M, Lanuti M, Faquin WC, Sadow PM, Tille JC, Intidhar Labidi-Galy S, Garris CS, Hugues S, Petrova TV, Ludewig B, Quezada S, Luther S, Mempel TR, Ciriello G, Pai SI, Michielin O, Böttcher JP, Weissleder R, Pittet MJ
Positioning and reversible suppression of CCR7+ dendritic cells in perivascular tumor niches shape cancer immunity. Immunity. 2025;59(1):161-176.e12 - PMID: 41421339 - PMCID: PMC12882814 - DOI: 10.1016/j.immuni.2025.11.020Garris C, Dunn GP, Weissleder R
Targeting myeloid cell polarization to prevent GBM recurrence. Mol Ther. 2025;34(1):41-43 - PMID: 41421347 - DOI: 10.1016/j.ymthe.2025.12.019Kaiser Y, Garris CS, Marinari E, Kim HS, Oh J, Pedard M, Halabi EA, Choi M, Parvanian S, Kohler R, Migliorini D, Weissleder R
Targeting immunosuppressive myeloid cells via implant-mediated slow release of small molecules to prevent glioblastoma recurrence. Nat Biomed Eng. 2025;:ePub - PMID: 41125869 - DOI: 10.1038/s41551-025-01533-2van Solinge TS, Oh J, Abels E, Koch P, Breakefield XO, Weissleder R, Broekman MLD
Probing the glioma micro-environment: analysis using biopsy in combination with ultra-fast cyclic immunolabeling. Neoplasia. 2024;57:101051 - PMID: 39270598 - PMCID: PMC11415813 - DOI: 10.1016/j.neo.2024.101051- More publications ...
News
We're excited to share that the Mass General Brigham Research Spotlight features CSB (Weissleder Lab) paper published in Nature Biomedical Engineering, “Targeting immunosuppressive myeloid cells via implant-mediated slow release of small molecules to prevent glioblastoma recurrence."
The work of Pittet Lab is featured in The Scientist - "Macrophages Play a Double Role in Cancer".
"Tumors talk to bones, and bones answer back" - Study by Engblom, Pfirschke et al. from the Pittet Lab is featured in Science and Nature. See also interview with the authors.
"Uncovering Cancer" - the work of Pittet Lab is featured in Nature Medicine article.
CSB work is profiled in MGH Research Institute spotlight "Mass General Researchers Investigate the ‘Big Eaters’ of the Immune System: #MacrophageMonday"