Study helps solve mystery of how sleep protects against heart disease
Researchers say they are closer to solving the mystery of how a good night’s sleep protects against heart disease. In studies using mice, they discovered a previously unknown mechanism between the brain, bone marrow, and blood vessels that appears to protect against the development of atherosclerosis, or hardening of the arteries—but only when sleep is healthy and sound.
The discovery of this pathway underscores the importance of getting sufficient, quality sleep to maintain cardiovascular health and could provide new targets for fighting heart disease, the leading cause of death among women and men in the United States, the researchers said. Their study, funded by the National Heart, Lung, and Blood Institute, part of the National Institutes of Health, appeared in the journal Nature.
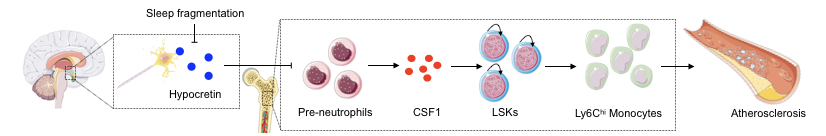
“We’ve identified a mechanism by which a brain hormone controls production of inflammatory cells in the bone marrow in a way that helps protect the blood vessels from damage,” explained Filip Swirski, Ph.D., the study’s lead author who also is an associate professor at Harvard Medical School and Massachusetts General Hospital. “This anti-inflammatory mechanism is regulated by sleep, and it breaks down when you frequently disrupt sleep or experience poor sleep quality,” he added.
Swirski noted that while other similar mechanisms may exist, the findings are nonetheless exciting. Recent research has linked sleep deficiency and certain sleep disorders, such as sleep apnea, to an increased risk of obesity, diabetes, cancer, as well as heart disease. But scientists have known little about the cellular and molecular underpinnings that could help explain the link between sleep and cardiovascular health.
Now, said Swirski, “we have a small piece of a larger puzzle.”
Poor or insufficient sleep is a major public health problem affecting millions of people of all ages. Studies show that getting enough quality sleep at the right times is vital for health, but fewer than half of adults in the United States get the recommended seven to eight hours per day.
To learn more about the impact of this deficiency on cardiovascular disease, the researchers focused on a group of mice that were genetically engineered to develop atherosclerosis. They disrupted the sleep patterns of half the mice and allowed the other half to sleep normally.
Over time, the mice with disrupted sleep developed progressively larger arterial lesions compared to the other mice. Specifically, the sleep-disrupted mice developed arterial plaques, or fatty deposits, that were up to one-third larger than the mice with normal sleep patterns. The sleep-disrupted mice also produced twice the level of certain inflammatory cells in their circulatory system than the control mice—and also lower amounts of a hypocretin, a hormone made by the brain that is thought to play a key role in regulating sleep and wake states.
The researchers also showed that sleep-deficient, atherosclerotic mice that received hypocretin supplementation tended to produce fewer inflammatory cells and develop smaller atherosclerotic lesions when compared to mice that did not get the supplementation. These results, they said, demonstrate that hypocretin loss during disrupted sleep contributes to inflammation and atherosclerosis. But they cautioned that more studies are needed, particularly in humans, to validate these findings and especially before experimenting with hypocretin therapeutically.
Still, health experts say, targeting the newly discovered biological mechanism—a so-called neuro-immune axis—could be a breakthrough that one day leads to new treatments for heart disease, sleep, and other disorders.
“This appears to be the most direct demonstration yet of the molecular connections linking blood and cardiovascular risk factors to sleep health,” said Michael Twery, Ph.D., director of the National Center on Sleep Disorders Research at NHLBI. Circadian biology refers to the 24-hour internal body clock that governs the expression of many genes in most every tissue and the regulation of sleep and wake.
“Understanding the potential impact of poor sleep and circadian health on the aging of blood cells and vascular disease opens new avenues for developing improved treatments,” Twery added.
This work was supported in part by NHLBI grants R35 HL135752, R01 HL128264, P01 HL131478, and NIH grant R35 HL139598. The study was also supported by additional institutions outside of NIH, including the American Heart Association. For a more complete funding disclosure, please see the full research article.
Article
McAlpine CS, Kiss MG, Rattik S, He S, Vassalli A, Valet C, Anzai A, Chan CT, Mindur JE, Kahles F, Poller WC, Frodermann V, Fenn AM, Gregory AF, Halle L, Iwamoto Y, Hoyer FF, Binder CJ, Libby P, Tafti M, Scammell TE, Nahrendorf M, Swirski FK
Sleep modulates haematopoiesis and protects against atherosclerosis
Nature. 2019; DOI: 10.1038/s41586-019-0948-2
Press Coverage
Listen to 14 February 2019: Atherosclerosis and disruptive science from Nature Podcast in Podcasts
WBUR (Boston NPR Stations) news
Poor sleep could clog your arteries. A mouse study shows how that might happen – Science
Taking Sleep to Heart – Harvard Medical School
Mass. General study finds how getting enough sleep reduces cardiovascular disease risk – EurekaAlert!
A good night’s sleep can cut heart disease risks: Short nights let harmful plaques build up in blood vessels, study finds – Daily Mail
Here’s How Poor Sleep May Hurt Your Heart – LiveScience
How Sleep Fights Inflammation & Disease, According To New Science – mindbodygreen
Real Reason Why Not Getting Enough Sleep Hurts Your Heart – International Business Times
Científicos de Harvard descubren cómo el sueño protege el corazón – La Vanguardia (Spain)
Amerikai kutatók közelebb kerültek annak a rejtélynek a megfejtéséhez, hogy miként védi a szívet egy jó éjszakai alvás – hvg.hu (Hungary)