Power to the T cells: A recipe to improve cancer immunotherapy
Therapies targeting T cell inhibitory checkpoint signaling pathways are redefining cancer survivability by providing durable responses to common cancer types at unprecedented rates. Yet only a minority of patients respond to these treatments, and evidence suggests that therapeutic benefit is achieved preferentially in patients with pre-existing tumor-infiltrating CD8+ T cells. Whether checkpoint blockade therapy can also benefit patients whose tumors are poorly (or not) infiltrated by T cells requires study.
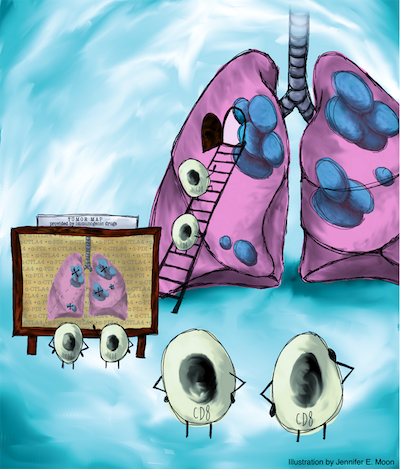
Here, Pfirschke, Engblom et al. aimed to address the following questions: Can we identify therapeutic strategies that convert ‘cold’ tumor tissues into immunologically ‘hot’ T cell-rich environments and promote antitumor CD8+ T cell immunity? Can we harness T cell tumor infiltration and the microenvironment to sensitize tumors to checkpoint therapy and durably control disease?
To answer these questions they explored and manipulated genetically engineered lung adenocarcinoma mouse models that are inadequately infiltrated by CD8 T cells and resist all current therapeutic options. Tumors in these models are driven by Kras and P53 mutations, which are common genetic drivers of the human disease. Lung cancer is the leading cause of cancer mortality worldwide.
First, Pfirschke, Engblom et al. evaluated drugs for their ability to induce immunogenic phenotypes in tumor cells in vitro and then tested the most promising candidate treatments in mice. These studies evaluated FDA-approved chemotherapeutics to favor clinical translatability. The most effective drugs (here, oxaliplatin combined with cyclophosphamide for lung tumors expressing Kras and P53 mutations) not only induced immunogenic phenotypes on tumor cells in vitro and in vivo but also provoked CD8 T cell infiltration into tumor areas. At a mechanistic level, the study identified that the antitumor immune response is complex because it is not only triggered by direct drug actions on tumor cells, but also relies on both innate and adaptive immune cells.
Second, Pfirschke, Engblom et al. found that drug-induced T cell recruitment into lung tumors successfully sensitized these tumors to checkpoint inhibition in that the combinatorial treatment was able to durably control lung cancer progression. Furthermore, immunogenic chemotherapy sensitized mice to checkpoint blockade inhibitors in models of murine fibrosarcoma and colon carcinoma, indicating that the findings are applicable to diverse tumor types.
Together, the data demonstrate that drugs selected for their ability to induce tumor immunogenicity can be used to transform ‘cold’ tumor tissues into immunologically ‘hot’ T cell-rich environments, which then become responsive to immune checkpoint therapy.
These findings have exciting implications for current and future clinical efforts that aim to expand the proportion of patients who respond to immune checkpoint therapy. Several scenarios can be considered to achieve tumor sensitization and improved outcomes in patients. First, it appears important to reevaluate the chemotherapeutics used in combination with checkpoint blockade agents to specifically include immunogenic drugs. The chemotherapeutics currently used against lung cancer might be insufficiently immunogenic. Replacing these drugs with more immunogenic compounds might expand the proportion of cancer patients who respond to current immune checkpoint treatments. Second, a precision medicine approach involving drug screening for individual patients may permit to select drugs with highest immunogenic activity in a given patient. This strategy is more technically challenging, but might benefit even more patients. Regardless of the approach, drugs that are already FDA-approved could be used to accelerate clinical translation.
Pfirschke C, Engblom C, Rickelt S, Cortez-Retamozo V, Garris C, Pucci F, Yamasaki T, Poirier-Colame V, Newton A, Redouane Y, Lin YJ, Wojtkiewicz G, Iwamoto Y, Mino-Kenudson M, Huynh TG, Hynes RO, Freeman GJ Kroemer G, Zitvogel L, Weissleder R, Pittet MJ
Immunogenic Chemotherapy Sensitizes Tumors to Checkpoint Blockade Therapy
Immunity. 2016;44:1-12