Identifying high grade dysplasia and invasive early pancreatic cancers may just have become easier
The detection of intraductal papillary mucinous neoplasms (IPMN), cystic tumor of the pancreas, is rising due to the increasing use and improved quality of cross-sectional imaging. IPMN evolve from low-grade dysplasia (LG) to high-grade dysplasia (HG) to invasive carcinoma (Inv/HG) and this progression is believed to account for up to a quarter of all pancreatic cancers. The timing and frequency of malignant progression is unknown, and therefore the management of patients remains controversial. This is in large part because current laboratory, endoscopic, cytologic, and imaging technologies are unable to reliably distinguish between low and high risk IPMN. Continued surveillance results in an enormous cost given the existing number of patients with incidentally-discovered pancreatic cysts and the fact that incidence increases with age.
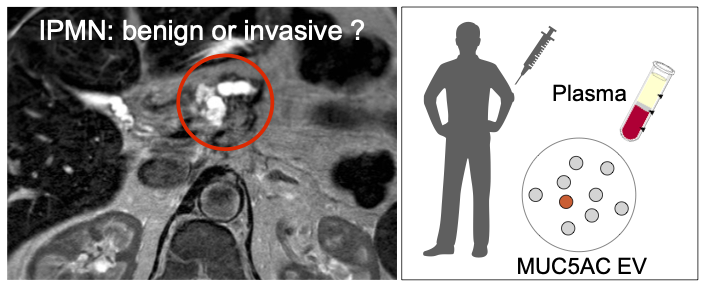
Researchers from the Weissleder lab in the Center for Systems Biology at MGH and the Departments of Surgery, Pathology and Radiology teamed up to develop a blood-based test. They hypothesized that analysis of circulating extracellular vesicles (EV) originating from (pre)malignant cells represents an opportunity for detecting the earliest forms of cancers. They developed an ultra sensitive, digital EV screening technology (DEST) optimized for the analysis of scant surface and intravesicular EV proteins. Using this method, they measured a number of putative protein biomarkers (MUC1, MUC2, MUC4, MUC5AC, MUC6, Das-1, STMN1, TSP1, TSP2, EGFR, EpCAM, GPC1, WNT-2, EphA2, S100A4, PSCA, MUC13, ZEB1, PLEC1, HOOK1, PTPN6, and FBN1) in 133 patients. The researchers identified MUC5AC as a predictive biomarker of high grade/invasive IPMN (sensitivity of 92%, specificity of 100%). The addition of MUC5AC as a biomarker to imaging and nomograms allowed detection of all cases requiring surgery, whereas imaging and nomograms alone would have missed 5/14 cases (36%).This new approach has the potential to improve the management and follow-up of patients with IPMN including avoiding unnecessary surgery.
Extracellular vesicle analysis allows for identification of invasive IPMN
Yang KS, Ciprani D, O’Shea A, Liss A, Yang R, Fletcher-Mercaldo S, Mino-Kenudson M, Castillo CF, Weissleder R.
Published in Gastroenterology on December 7, 2020 (PMID: 33301777)