A Precision Medicine Approach to Nanomedicine: New Method Developed to Predict Response to Nanotherapeutics
Researchers use MR imaging with magnetic nanoparticles to predict which tumors may be more responsive to therapeutic nanoparticles.
Many nanotherapeutics are currently being tested in clinical trials and several have already been clinically approved to treat cancers. But the ability to predict which patients will be most responsive to these treatments has remained elusive. Now, a collaboration between investigators at Massachusetts General Hospital (MGH) and Brigham and Women’s Hospital (BWH) has led to a new approach that uses an FDA-approved, magnetic nanoparticle and magnetic resonance imaging (MRI) to identify tumors most likely to respond to drugs delivered via nanoparticles. The team’s preclinical results are published in Science Translational Medicine November 18.
“Just as genetics is used in some cases to predict an individual’s response to a drug, we wanted to develop a companion diagnostic that can predict response based on physiological differences,” said Miles Miller, PhD, a postdoctoral fellow at the MGH Center for Systems Biology. “We hypothesized that ferumoxytol – a product that has been approved for the treatment of anemia – could be used to identify tumors that are more likely to respond to a nanomedicine.”
“Our goal is to develop new nanotherapeutics that can be safely and effectively delivered to cancer patients,” said Omid Farokhzad, MD, director of the Laboratory of Nanomedicine and Biomaterials at BWH. “One of the key translational challenges has been to better match patients to new nanotherapeutics based on patients’ physiology. Our work takes a precision medicine approach to nanotherapeutics: using this technique, we can predict how well drug-loaded nanoparticles will accumulate in a particular tumor.”
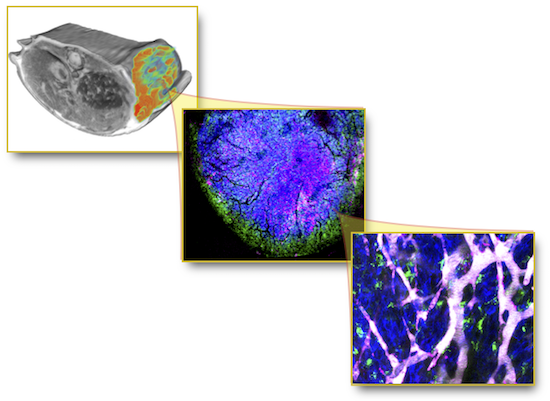
Farokhzad — who has founded three companies, all of which have nanomedicines in the clinic or fast-approaching clinical trials — teamed up with Ralph Weissleder, MD, PhD, Director of the MGH Center for Systems Biology and an expert in high-resolution in vivo imaging. The researchers hypothesized that the accumulation of nanoparticles may vary from patient to patient based on an individual’s unique physiology. For instance, some patients may harbor tumors with more “leaky” vasculature or other physiological conditions that allow nanoparticles to accumulate faster at tumor sites. This accumulation of nanoparticles within tumors is known as the enhanced permeability and retention (EPR) effect. To determine if it would be possible to predict which tumors have high or low EPR, the investigators used ferumoxytol in mouse models of solid tumor cancers. Because it is magnetic, ferumoxytol can be imaged using MRI.
“Clinical impact is the ultimate goal of our work. Therefore, we tested an imaging technology, MRI, commonly used in the clinic and a diagnostic nanoparticle, ferumoxytol, that is already FDA-approved for other indications,” said Weissleder, who is also an Attending Clinician in Interventional Radiology at MGH.
In addition to using MRI, the team labeled the magnetic nanoparticles with a fluorescent dye, allowing them to see the accumulation of particles on a single-cell level by microscopy.They categorized each tumor as having “low,” “medium” or “high” EPR and then treated each tumor with a chemotherapeutic drug delivered via nanoparticles.
The researchers report that in preclinical models, their MR imaging strategy accurately predicted how much drug would reach the tumors (with more drug being delivered to tumors with higher EPR) and therefore how well the tumors would respond to the drug-loaded nanoparticles.
“This work represents a major stepping stone toward translating new discoveries of nanotherapeutics into clinical impact and selecting patients for nanotherapeutic trials,” said Farokhzad.
To continue moving this work closer to clinical validation, the team intends to perform similar studies in patients. Studies of different forms of cancer may also help the team to identify which cancer types will be most responsive to nanotherapeutics.
Miller MA, Gadde S, Pfirschke C, Engblom C, Sprachman MM, Kohler RH, Yang KS, Laughney AM, Wojtkiewicz G, Kamal N, Bhonagiri S, Pittet MJ, Farokhzad OC, Weissleder R
Predicting therapeutic nano- medicine e cacy using a companion MR imaging nanoparticle.
Sci. Transl. Med. 7, 314ra183 (2015).
Press Coverage
Nanomedicine gets personal – Science Translational Medicine
New Technique Could Help Personalize Nanomedicine – Chemical & Engineering News